When you hear the words “cancer” and “women,” pink ribbons probably pop into your mind — the ubiquitous symbol of the fight against breast cancer. For years it’s been a high-profile and well-supported disease, and the result shows in the myriad of detection methods and treatments now available. Not so for ovarian cancer, which ranks fifth in cancer deaths among women, accounting for more deaths than any other cancer of the female reproductive system.
According to the American Cancer Society, approximately 22,340 new cases of ovarian cancer were diagnosed in 2007. An estimated 15,280 American women died from the disease last year. Why the high death rate? Because to date, there is no early detection method that will accurately predict or identify ovarian cancer in its beginning stages, when the survival rate is much higher. If the cancer has not spread
outside the ovary, the five-year survival rate is 93 percent. However, only 19 percent of all ovarian cancers are found at this stage.
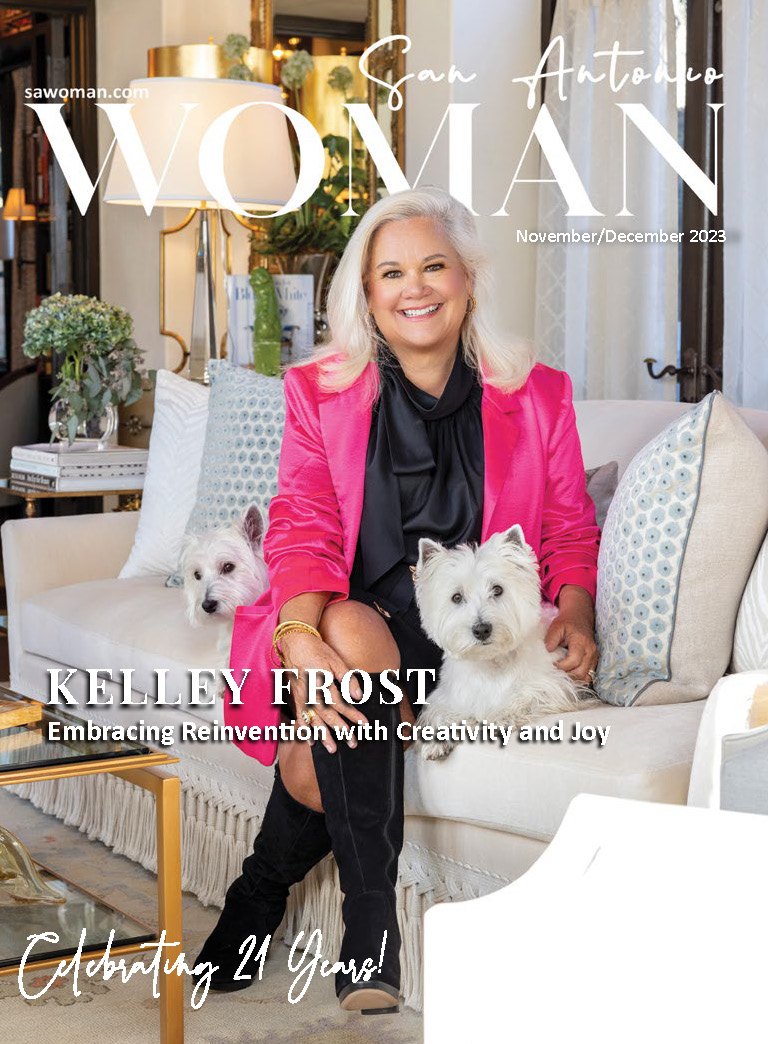
That’s why SAN ANTONIO WOMAN is doing its part in raising awareness of the risk factors, as well as symptoms of ovarian cancer.
RISK FACTORS:
Age: Most ovarian cancers happen after menopause. Around two-thirds of women who get ovarian cancer are 55 or older.
Race: Ovarian cancer is more prevalent in Caucasian women than African- American women.
Obesity: An American Cancer Society study found a higher rate of ovarian cancer in women who were overweight. The risk went up 50 percent in the heaviest women.
Menstrual periods: There appears to be a link between the number of periods in a woman’s lifetime and her risk of getting ovarian cancer. Women who started their periods before the age of 12, and/or went through menopause after the age of 50, have a small increased risk of ovarian cancer.
Family history: Ovarian cancer risk is higher in women whose close blood relatives (mother, sister, daughter) have, or had, this disease. There is a higher risk if ovarian cancer occurred at an early age.
Breast cancer: Women who have had breast cancer have a higher risk of ovarian cancer.
“There are no tests or follow-up strategies that can reliably detect ovarian cancer early,” says Dr. Tyler Curiel, executive director of the Cancer Therapy & Research Center at the University of Texas Health Science Center at San Antonio. “Women at high risk (with known BRCA gene mutations, or with a mother, sister or daughter who had ovarian or breast cancer before the age of 40) should discuss their options for evaluation, follow-up and risk reduction with an expert in ovarian cancer.” He also recommends high-risk
women could consider enrolling in a prospective research study.
LISTEN TO YOUR BODY
One of the myths associated with ovarian cancer is that it’s a silent killer. This is not true. In fact, it whispers, but we have to be listening to our bodies to hear it. That’s why raising awareness of the symptoms associated with ovarian cancer is so important.
If you have any of the following symptoms, report them to your doctor:
Swelling of the stomach
Unusual vaginal bleeding
Pelvic pressure
Back or leg pain
Problems such as gas, bloating, long-term stomach pain, constipation or indigestion
A feeling of fullness rapidly after eating
Women with ovarian cancer report that symptoms are persistent and represent a change from normal for their bodies. The frequency and/or number of such symptoms are key factors in the diagnosis of ovarian cancer. Several studies show that even early stage ovarian cancer can produce these symptoms.
BE YOUR OWN ADVOCATE
Admittedly, the symptoms of ovarian cancer are vague and nonspecific. Often women ignore them, or if they do see a physician, the doctor may not give these kinds of complaints the attention they deserve. Women who have these symptoms almost daily for more than a few weeks should see a gynecologist. Prompt medical evaluation may lead to detection at the earliest possible stage of the disease.
DIAGNOSIS AND TREATMENT
If you have the signs and symptoms that are suggestive of ovarian cancer, your doctor will probably perform three tests, including:
Pelvic exam — To feel for growths or other abnormalities. Experts recommend this exam be done annually.
Transvaginal or pelvic ultrasound — Sound waves are used to create a picture of the ovaries and can reveal if there are masses on the ovaries.
CA-125 blood test — This tests for a substance in the blood that may increase when a cancerous tumor is present.
It’s important to note that none of these tests is definitive when used alone. They are most effective when used in com- bination with each other. Your doctor may also use other imaging tests, such as CT or PET scan as part of the diagnostic process.
Dr. Curiel says evaluating nonspecific symptoms can be tricky. “A false positive result could precipitate unnecessary surgery. A false negative could miss an early cancer,” he cautions. “Patients and their health care providers have to analyze the clinical situation from many angles, including all known risk factors, to decide how to evaluate nonspecific symptoms.”
The only definitive way to determine if a patient has ovarian cancer is through surgery and biopsy.
Approximately 90 percent of cases occur in the epithelium, the thin layer of tissue that covers the ovaries. “Epithelial ovarian cancer is usually treated with optimal surgical debulking, plus combination chemotherapy,” says Dr. Curiel.
Multiple studies conducted over the past decade have shown that survival is markedly improved when a gynecological oncologist performs the debulking surgery. This is attributed to these specialists’ tendency to perform more aggressive surgical techniques that in turn realize better outcomes.
Author: Kelly A. Goff








0 Comments