New Research Drives Improvements in Cervical Cancer Treatment
By Paul J. Watkins
According to the American Cancer Society, invasive cancer of the cervix is diagnosed in the United States in 14,480 women annually. Each year, about 4,290 of those women will die from cervical cancer. Every year, 500,000 women worldwide will receive a cervical cancer diagnosis.
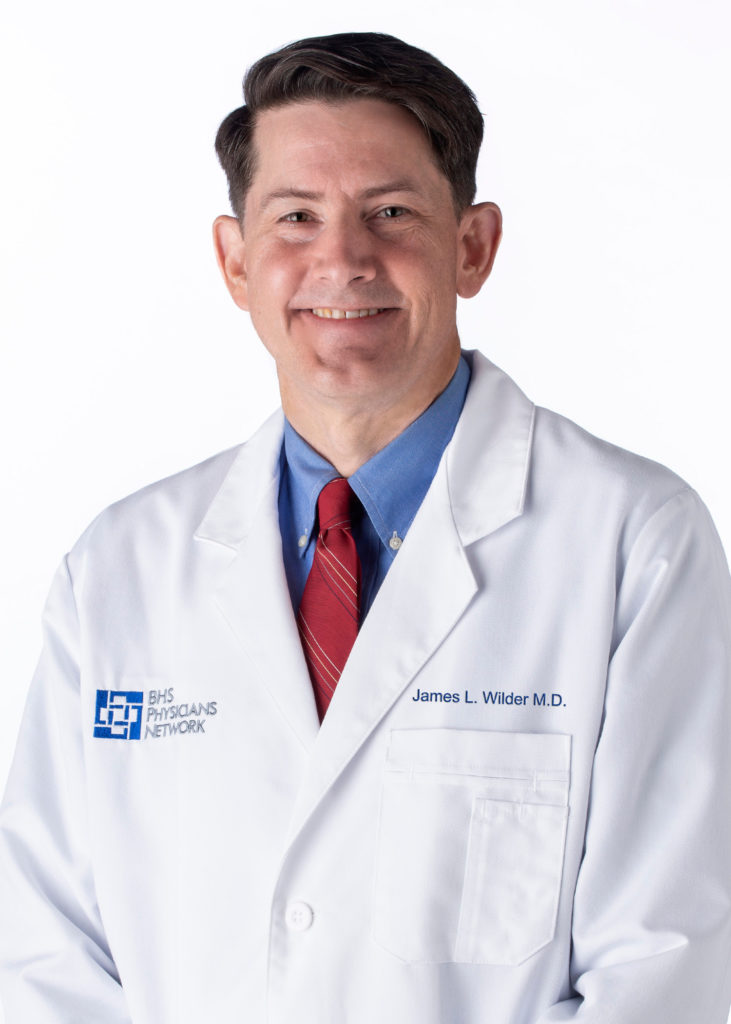
James L. Wilder, M.D., ABOG, board-certified gynecological oncology surgeon at South Texas Gynecologic Oncology in San Antonio, says that current research into cervical cancer has produced breakthroughs that are changing the way gynecological oncology surgeons treat the disease. “Up until about a year and a half ago, I was doing all my surgery for early-stage cervical cancer laparoscopically. Then, a phase III randomized control trial published in the New England Journal of Medicine (NEJM) showed that laparoscopic surgery patients would recur at a higher rate four years later compared to those who had surgery through an open incision. Other studies supported this and the National Comprehensive Cancer Network (NCCN), as well as the SGO (Society of Gynecologic Oncology), now recommend a laparotomy (abdominal incision) be considered for most cervical cancer patients (stages IA2-IB). So we changed back to treating our early-stage cervical cancer patients with open surgery.”
“For more advanced cervical cancer in a recurrent/metastatic setting, immunotherapy was added as a preferred treatment in 2017, based on a Keynote Trial,” continues Dr. Wilder. “Immunotherapy has really been a game-changer because these women who were probably going to die – within a year sometimes – are just not dying. I’m not saying they’re getting cured, because the cancer is not going away; but they’re living longer.” Dr. Wilder adds that angiogenesis inhibitors are another treatment option; they stop blood vessel growth, which cervical cancers need to continue to grow and metastasize.
“In addition to immunotherapies, there are some antibody-drug conjugates (ADCs) which are also hopeful to improve the opportunities for treatment,” states Joseph de la Garza, M.D., FACOG, a board-certified gynecological oncology surgeon at Texas Oncology in San Antonio. ADCs target and kill tumor cells while leaving healthy cells untouched. “This is a new approach that’s approved as a second-line therapy for metastatic cervical cancer. The largest component of research is to move away from standard chemotherapies and to look at immunotherapies and other novel agents, which can improve response rates and opportunities for cure.”
Dr. Wilder says that other than the surgical methods gynecological oncology surgeons use, the standard of care treatment for cervical cancer (except in earliest stages) remains a combination of radiation and chemotherapy. “We use surgery for the microscopic, earliest diseases and some of the disease that you can see with the naked eye – but the cancer has to basically be an inch in size. When the cervical cancer is larger, we start using radiation and chemotherapy.”
“The backbone of treatment for cervical cancer for the longest period of time has been radiation. You give what’s called ‘external radiation’ from the outside, and then you give what’s called ‘internal radiation,’ or ‘brachytherapy,’ from the inside. This is combined with the chemotherapy. That’s the current standard of treatment for the majority of cervical cancers.”
The good news is that cervical cancer can be stopped before it begins. “If caught at the precancerous stage, cervical cancer can be completely prevented,” says Dr. de la Garza. “So, it’s not cured, it’s prevented, which is key. But similar to all cancers, the opportunity for a cure decreases as you progress in stages. At precancerous stages, it can be prevented. At early stages, there’s a higher opportunity for cure. At later stages, it becomes more difficult to achieve cure.”
The majority of cervical cancer is caused by the human papillomavirus (HPV). Vaccines are available to protect against HPV, and Dr. de la Garza adds that improving the uptake of vaccines is highly effective in preventing cervical cancer. “The best therapy that I can give someone for a cancer is to prevent them from ever getting it. The vaccines have been around for many years. They have previously been what’s called ‘quadrivalent,’ which means they protected against four strains of HPV. Now, they’re what’s called ‘nonavalent,’ so they provide protection against nine strains of HPV.
“Increasing the acceptance, distribution, and receipt of these vaccines in our children is really what’s going to make the largest impact,” informs Dr. de la Garza. “Treating second-line, metastatic cervical cancer only helps a handful of patients for a short period of time. But if I can prevent future generations from even acquiring HPV, that’s going to be my biggest impact.”
To contact the physicians interviewed in this article, visit:
For additional resources, visit the American Cancer Society website:









0 Comments