by Paul Watkins
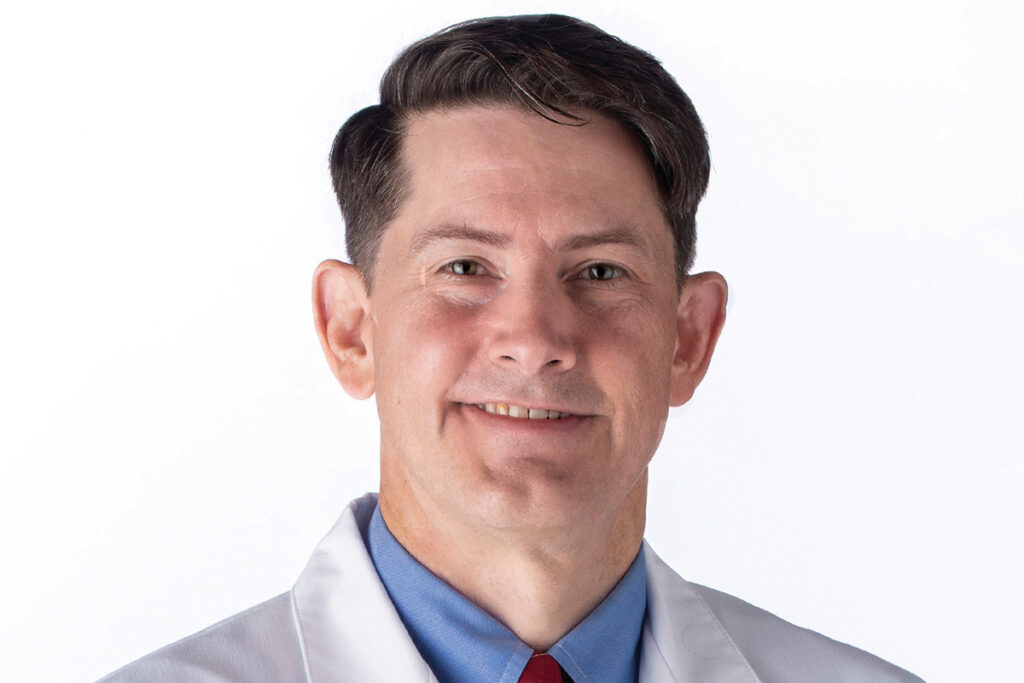
“In the United States, the gynecologic cancer that’s most commonly on the rise is endometrial cancer, which is a form of uterine cancer,” says James L. Wilder, M.D., a board-certified gynecological oncology surgeon at South Texas Gynecologic Oncology in San Antonio. “In absolute numbers, they’re all increasing, mostly likely as a result of population increases. However, what we’re actually seeing more of, in percentages, is endometrial cancer – and specifically advanced endometrial cancer.”
Dr. Wilder says there are certain symptoms that women should be aware of that can indicate the presence of endometrial cancer and should be brought to the attention of a physician. The most common symptom is bleeding in a post-menopausal woman, he informs, and the vast majority of time, it’s in the form of spotting.
The surgeon says women may ignore this symptom because they’re not convinced that it’s coming from the vagina. It happens when they urinate, and it’s hard to tell where it came from. They think it may be a hemorrhoid, and there’s very, very little blood on the toilet paper when they wipe. Dr. Wilder emphasizes that any abnormal bleeding in a post-menopausal female should make a physician consider the possibility of endometrial cancer.
“It’s true that most endometrial or uterine cancer occurs in the post-menopausal female age group. It can occur, though with less frequency, in someone who’s not in menopause yet, and that will generally take the form of any type of abnormal bleeding. Let’s say a woman in her twenties or thirties is having periods twice a year, or not at all. Just because she hadn’t bled for a year and she’s in her twenties doesn’t mean she’s in menopause. Maybe she has a dysfunction of her ovaries, where she’s not ovulating. Any kind of abnormal bleeding before menopause has to make you look at endometrial cancer. Though women in their twenties and thirties isn’t the most prevalent age group in which you see endometrial cancer, it does occur.
“There’s only one very reliable screening test for any female cancer, and that’s a Pap smear, which is used for identifying cervical cancer – often in its earliest stages – and it empowers women and their physicians to treat it very effectively. We’ve steadily seen a decline in the incidence of cervical cancer. It’s not one of the top cancers in the United States anymore. Unfortunately, it’s still in the top three killers of women worldwide.”
Dr. Wilder notes that there are no screenings available for endometrial or uterine cancer. This fact makes it that much more important for a woman experiencing symptoms not to delay seeing her physician. As with all cancers, the sooner it’s caught, the better the options for treating it.
“It’s true that most ovarian cancer cases have symptoms, but they’re not reliable,” he notes. “A lot of those symptoms overlap with other diseases, so when a woman comes in with a complaint of urinary frequency, shortness of breath, or irritable bowel symptoms, most doctors aren’t going to immediately clue in on the possibility of ovarian cancer. That’s probably not the first thought that crosses their mind.
“Early-stage endometrial cancer is almost always curable with surgery alone – a hysterectomy. That is recommended for most women. There are exceptions if a woman is very young when her endometrial cancer is diagnosed, and maybe her cancer meets certain criteria – it’s not invading surrounding tissue, for example. A gynecological oncologic surgeon might recommend high-dose progesterone therapy until the woman is in remission and then she can try to conceive and have a child. Once that’s done, then the uterus comes out. For most women, though, the treatment is going to be a hysterectomy.
“In the advanced stages, hysterectomy is still part of the therapy, but almost always, the woman will also receive chemotherapy and/or radiation.”
Dr. Wilder notes that a new, exciting treatment was introduced within the last two years. It’s an immunotherapy drug that has been added to the frontline treatment of uterine cancer. “In addition to the chemotherapy, we’ll add an immunotherapy drug. I’m seeing women who should not have survived two years after their diagnosis – let’s say after a recurrence of advanced-stage disease. With immunotherapy, they’re being cured, which is something I’ve never seen before. I see that in advanced ovarian cancer as well, with the advent of immunotherapy and targeted therapy of different cancers. There is a tidal wave of people who have been cured of cancer. It’s really exciting for me to deliver immunotherapy and see those outcomes.”
For more information or to make an appointment, please call (210) 903-0677 or visit www.BaptistMedicalNetwork.com/OBGYNs.








0 Comments